Navigating the complexities of government assistance programs can be daunting, especially when it comes to understanding how they interact with each other. In this article, we delve into the relationship between food stamps, also known as Supplemental Nutrition Assistance Program (SNAP), and Medicaid, exploring how one can affect the eligibility and coverage of the other.
As we explore this topic, we’ll examine the impact of food stamp income and asset limits on Medicaid eligibility, discuss the concept of categorical eligibility, and highlight special considerations for individuals receiving both forms of assistance. By providing clear explanations and practical examples, we aim to empower readers with the knowledge they need to make informed decisions about their healthcare and nutritional support.
Eligibility
explanatoryFood assistance benefits can affect Medicaid eligibility in several ways:
Impact on Income Eligibility
- Food assistance benefits, such as SNAP (Supplemental Nutrition Assistance Program), can reduce a household’s countable income for Medicaid purposes.
- This is because SNAP benefits are considered a form of in-kind assistance, which is not counted as income when determining Medicaid eligibility.
- As a result, households that receive SNAP benefits may have lower countable incomes and qualify for Medicaid coverage.
Impact on Asset Eligibility
- Food assistance benefits can also affect a household’s countable assets for Medicaid purposes.
- In some states, households that receive SNAP benefits are allowed to have higher countable assets and still qualify for Medicaid.
- This is because SNAP benefits are considered a form of protected asset, which is not counted against the Medicaid asset limit.
Impact on Work Requirements
- In some states, households that receive food assistance benefits are exempt from certain Medicaid work requirements.
- This means that these households may be able to qualify for Medicaid coverage even if they do not meet the state’s work requirements.
Income Limits
Income limits play a significant role in determining eligibility for both food stamps and Medicaid. Exceeding the specified income thresholds can affect an individual’s or family’s ability to qualify for these programs.
To determine eligibility, both food stamps and Medicaid consider household income, which includes income from all sources, such as wages, self-employment, investments, and government benefits. However, the income limits for these programs differ.
Food Stamp Income Limits
Food stamp income limits vary depending on household size and composition. The gross income limit for a one-person household in 2023 is $1,500 per month, while the net income limit (after certain deductions) is $1,195 per month.
For larger households, the income limits increase. For example, a four-person household has a gross income limit of $2,829 per month and a net income limit of $2,272 per month.
Medicaid Income Limits
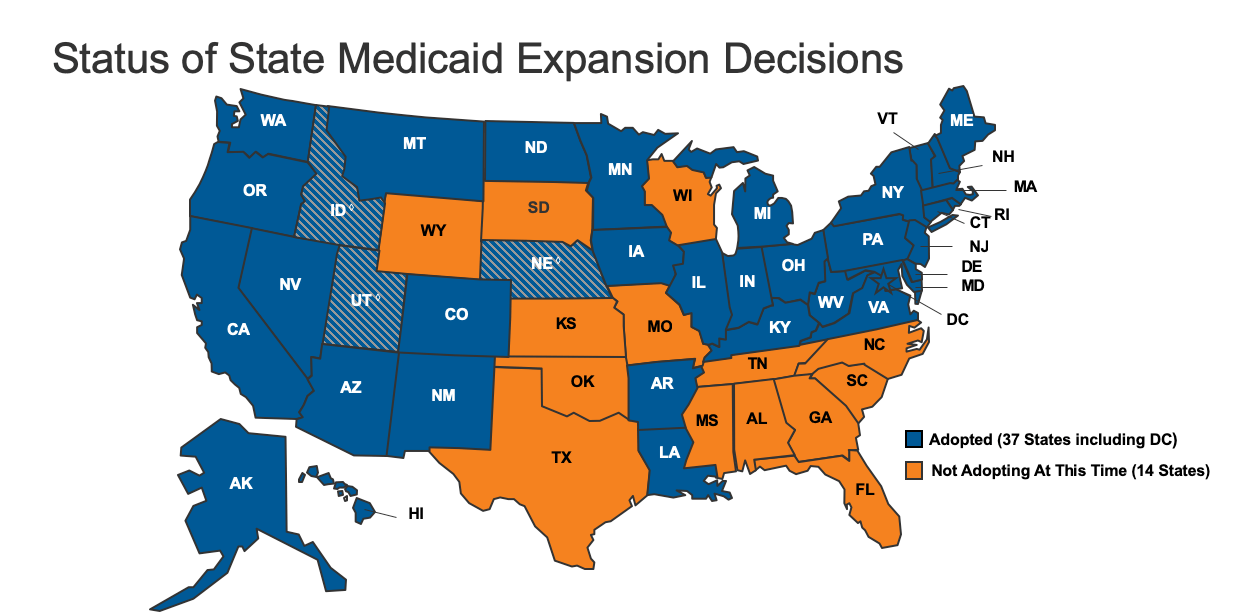
Medicaid income limits also vary by state, as each state sets its own eligibility criteria. In general, Medicaid income limits are higher than food stamp income limits.
For example, in California, the income limit for a one-person household is $1,766 per month in 2023, while the income limit for a four-person household is $3,533 per month.
Comparison of Food Stamp and Medicaid Income Limits
The following table compares the income limits for food stamps and Medicaid in California for a one-person household in 2023:
| Program | Gross Income Limit | Net Income Limit |
|---|---|---|
| Food Stamps | $1,500 | $1,195 |
| Medicaid | $1,766 | N/A |
As shown in the table, the Medicaid income limit is higher than the food stamp income limit. This means that some individuals who exceed the food stamp income limit may still be eligible for Medicaid.
Asset Limits
Asset limits are a crucial factor in determining Medicaid eligibility. Unlike income limits, which focus on your current earnings, asset limits consider the value of your possessions.
For individuals, the asset limit is generally set at $2,000. For couples, the limit is higher at $3,000. These limits include cash, bank accounts, stocks, bonds, and other financial assets. However, certain assets are exempt from these limits, such as your primary residence, one vehicle, and personal belongings.
Impact of Assets on Medicaid Coverage
Exceeding the asset limits can impact your Medicaid coverage in several ways:
- Ineligibility: If your assets exceed the limits, you may become ineligible for Medicaid.
- Spend-down period: If you exceed the asset limits but have high medical expenses, you may enter a spend-down period. During this period, you will need to spend down your assets to the limit before Medicaid coverage begins.
- Medicaid Estate Recovery Program (MERP): After your death, Medicaid may file a claim against your estate to recover the cost of services provided to you. This is only applicable if you received Medicaid long-term care services and had assets above the asset limits.
Categorical Eligibility
Categorical eligibility refers to the qualification for Medicaid based on certain categories of individuals, regardless of their income or assets. Food stamps, also known as Supplemental Nutrition Assistance Program (SNAP), can impact categorical eligibility for Medicaid.
Impact of Food Stamps on Categorical Eligibility
Individuals who receive food stamps are automatically eligible for Medicaid if they meet other eligibility criteria, such as age, disability, or pregnancy. This is because food stamps are considered an indicator of low income and financial hardship, which makes individuals more likely to qualify for Medicaid.
By receiving food stamps, individuals can meet the income requirements for Medicaid categorical eligibility, even if their income would otherwise be too high to qualify.
Special Considerations
Individuals receiving both food stamps and Medicaid may face unique challenges and require special considerations. Understanding these challenges and implementing appropriate solutions is crucial for ensuring their well-being.
One potential challenge is the income and asset limits for food stamps and Medicaid, which may differ. This can lead to situations where individuals qualify for one program but not the other. To address this, coordination between agencies and streamlined eligibility processes are essential to ensure that individuals receive the benefits they are entitled to.
Impact on Eligibility
Receiving food stamps can impact Medicaid eligibility in certain circumstances. For instance, if an individual’s income increases due to food stamp benefits, they may no longer qualify for Medicaid. Conversely, if food stamp benefits decrease, an individual may become eligible for Medicaid.
To mitigate these challenges, regular income and eligibility reviews are necessary to ensure that individuals receive the appropriate benefits based on their current circumstances.
Final Thoughts
In conclusion, the relationship between food stamps and Medicaid is complex and multifaceted. Understanding how one program can affect the other is crucial for individuals seeking comprehensive healthcare and nutritional support. By carefully considering the eligibility requirements, income and asset limits, and special considerations Artikeld in this article, readers can navigate the complexities of these programs and make informed choices that maximize their access to essential services.
FAQ Corner
Does receiving food stamps automatically qualify me for Medicaid?
No, receiving food stamps does not automatically qualify you for Medicaid. While some states use food stamp eligibility as a basis for determining Medicaid eligibility, others have different criteria and income limits.
How do food stamp income limits affect Medicaid eligibility?
In some states, exceeding the income limits for food stamps can impact Medicaid eligibility. Individuals with incomes above these limits may not qualify for Medicaid, even if they meet other eligibility criteria.
What is categorical eligibility for Medicaid?
Categorical eligibility refers to automatic Medicaid eligibility for certain groups of individuals, such as pregnant women, children, and individuals with disabilities. In some cases, receiving food stamps can affect categorical eligibility by meeting income and resource requirements.